[ad_1]
In inflammatory bowel disorder, mental stress can deliver two unpleasant responses
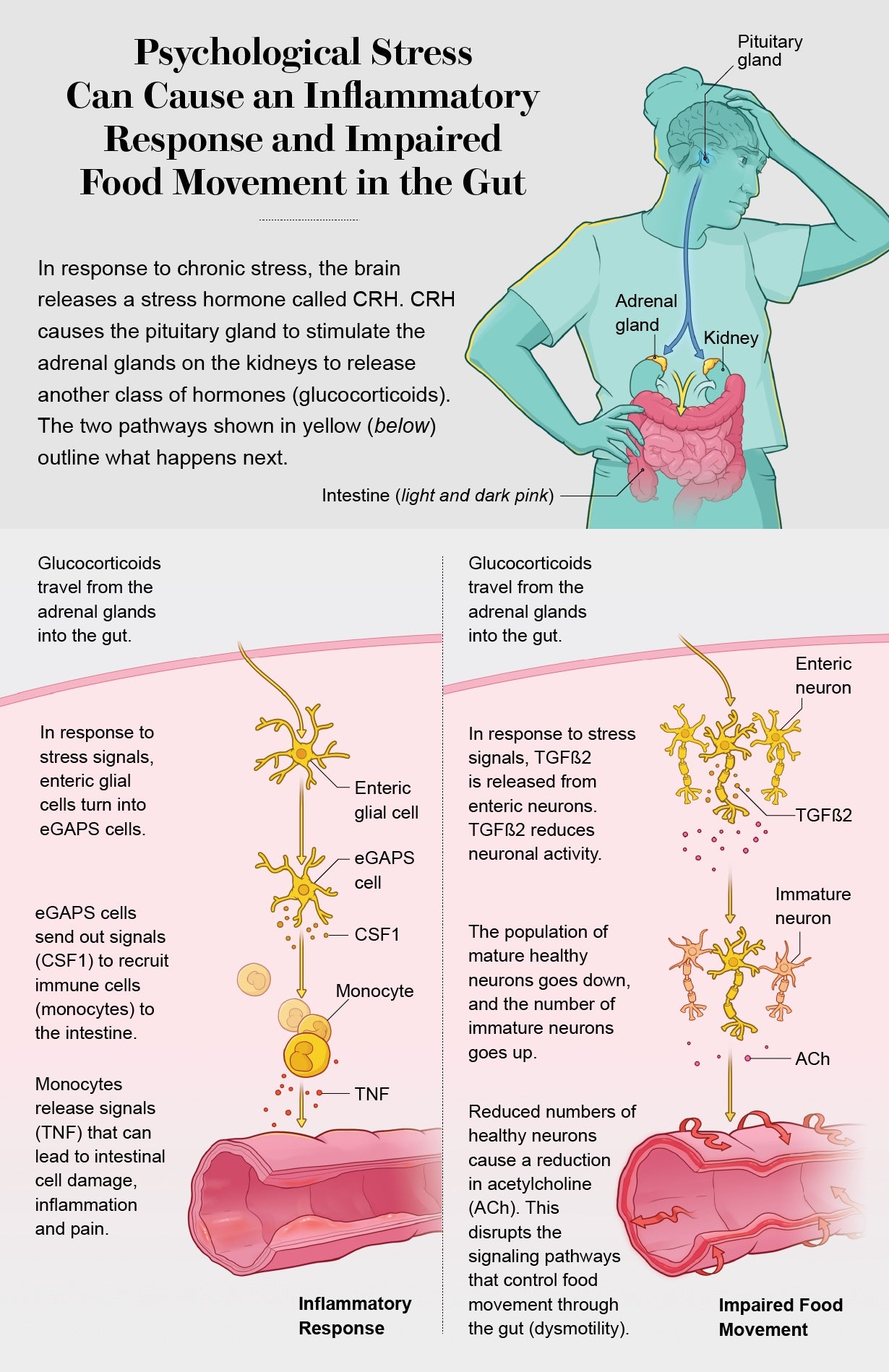
Bouts of disabling suffering, bleeding, weight decline and hospitalization that in some cases call for surgical treatment: which is the whole lot of about 3 million older people in the U.S. who experience from inflammatory bowel disease, or IBD. (The health issues has two major types, Crohn’s condition and ulcerative colitis. It is usually affiliated with an overactive immune method and may possibly have a genetic component.) Solutions normally require some range of immunosuppressant these kinds of as a steroid drug. But even controlled instances have periodic flare-ups, and the causes have been tricky to pin down.
Now experts have traced two thorough molecular pathways from the mind to the gut that make IBD flares. And in a few various groups of IBD patients, they observed that psychological stress—a dying in the spouse and children or a bad combat with a liked 1, for instance—can cause the release of brain substances that lead to IBD symptoms. This will not suggest IBD is all in the head, emphasizes Christoph A. Thaiss of the University of Pennsylvania, a person of the researchers. But it does indicate psychotherapy and focused anxiety-management strategies have important—and until finally now underappreciated—roles to enjoy in stopping and treating agonizing flares.


This write-up was originally published with the title “The Mind-Gut Link” in Scientific American 329, 2, 86 (September 2023)
doi:10.1038/scientificamerican0923-86
[ad_2]
Resource backlink




